Menu
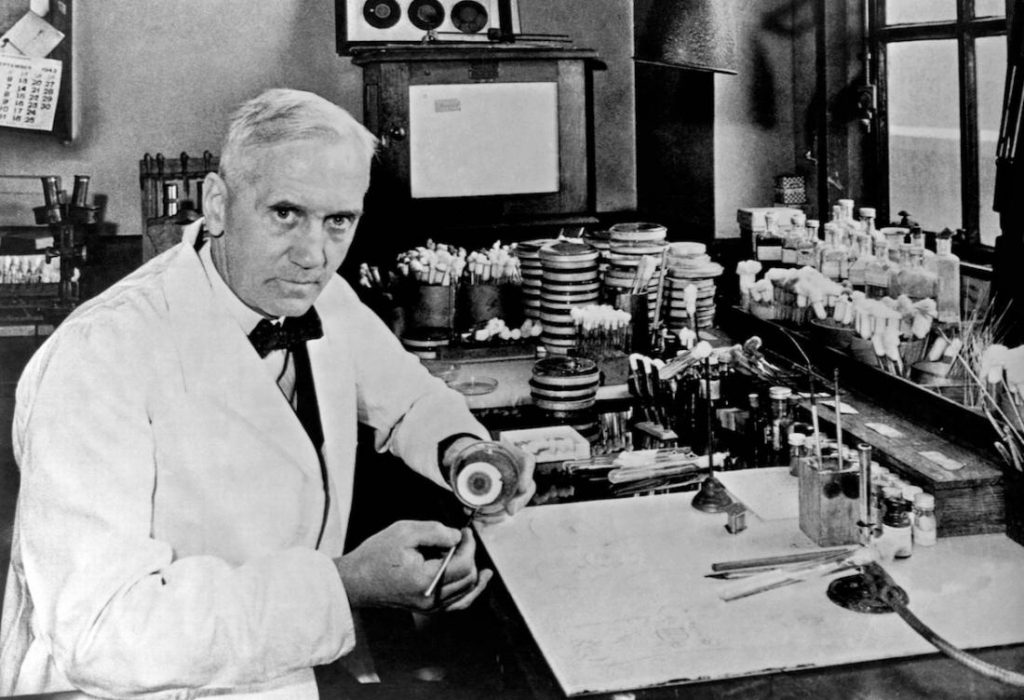
Sir Alexander Fleming, (6 August 1881 - 11 March 1955) was a Scottish biologist, pharmacologist and botanist who discovered Penicillin. (Photo by Universal History Archive/UIG via Getty Images)
that Alexander Fleming was born, on August 6, 1881, in Ayrshire, Scotland. He was the third of the four children of farmer Hugh Fleming (1816–1888) and his wife Grace Stirling Morton.
After working in a shipping office for four years, the twenty-year-old Fleming inherited some money from an uncle, John Fleming. His elder brother, Tom, was already a physician and suggested to him that he should follow the same career, and so in 1903, the younger Alexander enrolled at St Mary's Hospital Medical School in Paddington; he qualified with an MBBS degree from the school with distinction in 1906. Het joined the research department at St Mary's, where he became assistant bacteriologist to Sir Almroth Wright, a pioneer in vaccine therapy and immunology.
In 1908, he gained a BSc degree with Gold Medal in Bacteriology, and became a lecturer at St Mary's until 1914. Fleming served throughout World War I as a captain in the Royal Army Medical Corps, and was Mentioned in Dispatches. He and many of his colleagues worked in battlefield hospitals at the Western Front in France. In 1918 he returned to St Mary's Hospital, where he was elected Professor of Bacteriology of the University of London in 1928.
During World War I, Fleming witnessed the death of many soldiers from sepsis resulting from infected wounds. Antiseptics, which were used at the time to treat infected wounds, often worsened the injuries. In an article he submitted for the medical journal The Lancet during World War I, Fleming described an ingenious experiment, which he was able to conduct as a result of his own glass blowing skills, in which he explained why antiseptics were killing more soldiers than infection itself during World War I. Antiseptics worked well on the surface, but deep wounds tended to shelter anaerobic bacteria from the antiseptic agent, and antiseptics seemed to remove beneficial agents produced that protected the patients in these cases at least as well as they removed bacteria, and did nothing to remove the bacteria that were out of reach. Sir Almroth Wright strongly supported Fleming's findings, but despite this, most army physicians over the course of the war continued to use antiseptics even in cases where this worsened the condition of the patients.
At St Mary’s Hospital Fleming continued his investigations into antibacterial substances. Testing the nasal secretions from a patient with a heavy cold, he found that nasal mucus had an inhibitory effect on bacterial growth. This was the first recorded discovery of lysozyme, an enzyme present in many secretions including tears, saliva, skin, hair and nails as well as mucus. Although he was able to obtain larger amounts of lysozyme from egg whites, the enzyme was only effective against small counts of harmless bacteria, and therefore had little therapeutic potential.
When I woke up just after dawn on September 28, 1928, I certainly didn't plan to revolutionise all medicine by discovering the world's first antibiotic, or bacteria killer. But I suppose that was exactly what I did.
— Alexander Fleming
By 1927, Fleming had been investigating the properties of staphylococci. He was already well-known from his earlier work, and had developed a reputation as a brilliant researcher, but his laboratory was often untidy. On 3 September 1928, Fleming returned to his laboratory having spent August on holiday with his family. Before leaving, he had stacked all his cultures of staphylococci on a bench in a corner of his laboratory. On returning, Fleming noticed that one culture was contaminated with a fungus, and that the colonies of staphylococci immediately surrounding the fungus had been destroyed, whereas other staphylococci colonies farther away were normal, famously remarking "That's funny".
Fleming grew the mould in a pure culture and found that it produced a substance that killed a number of disease-causing bacteria. He identified the mould as being from the Penicillium genus, and, after some months of calling it "mould juice", named the substance it released penicillin on 7 March 1929.
He investigated its positive anti-bacterial effect on many organisms, and noticed that it affected bacteria such as staphylococci and many other Gram-positive pathogens that cause scarlet fever, pneumonia, meningitis and diphtheria, but not typhoid fever or paratyphoid fever, which are caused by Gram-negative bacteria, for which he was seeking a cure at the time. It also affected Neisseria gonorrhoeae, which causes gonorrhoea although this bacterium is Gram-negative.
Fleming published his discovery in 1929, in the British Journal of Experimental Pathology, but little attention was paid to his article. Fleming continued his investigations, and found that cultivating penicillium was quite difficult, and that after having grown the mould, it was even more difficult to isolate the antibiotic agent. Fleming's impression was that because of the problem of producing it in quantity, and because its action appeared to be rather slow, penicillin would not be important in treating infection. Fleming also became convinced that penicillin would not last long enough in the human body (in vivo) to kill bacteria effectively. Many clinical tests were inconclusive, probably because it had been used as a surface antiseptic.
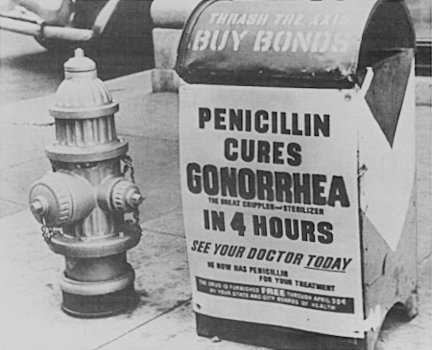 In the 1930s, Fleming’s trials occasionally showed more promise, and he continued, until 1940, to try to interest a chemist skilled enough to further refine usable penicillin. Fleming finally abandoned penicillin, and not long after he did, Howard Florey and Ernst Boris Chain at the Radcliffe Infirmary in Oxford took up researching and mass-producing it, with funds from the U.S. and British governments. They started mass production after the bombing of Pearl Harbor. By D-Day in 1944, enough penicillin had been produced to treat all the wounded in the Allied forces.
In the 1930s, Fleming’s trials occasionally showed more promise, and he continued, until 1940, to try to interest a chemist skilled enough to further refine usable penicillin. Fleming finally abandoned penicillin, and not long after he did, Howard Florey and Ernst Boris Chain at the Radcliffe Infirmary in Oxford took up researching and mass-producing it, with funds from the U.S. and British governments. They started mass production after the bombing of Pearl Harbor. By D-Day in 1944, enough penicillin had been produced to treat all the wounded in the Allied forces.
Fleming was said to be "a reticent and rather taciturn man, with great independence of mind and strength of character". He was a keen observant of nature and everything around him, always ready to devise and test new methods for studying germs in the lab. He accepted the many honors that were bestowed upon him with modesty. It seemed that simple tributes touched him most, such as the letter of some poor person who had benefitted from penicillin.
Fleming died on 11 March 1955, at his home in London of a heart attack. He was buried in St Paul's Cathedral